THE HEART OF AN ATHLETE
Exercise causes a number of changes to the body. Acutely, it results in increased cardiac output (more blood flow), increased blood pressure, decreased peripheral vascular resistance (think of this as dilation of the capillaries at the level of your organs to allow for even more enhanced blood flow), and increased oxygen delivery. Longterm effects of exercise result in structural modifications of the heart, and these changes are most recognizable in male athletes who have been undergoing endurance training.
Generally speaking, regardless of gender, about 1 out of 2 athletes will show some evidence of changes in the heart with training. These changes are termed “cardiac remodeling.” Studies indicate that 1 out of 8 athletes will show a significant increase in the size of the left ventricle (the major pumping chamber of the heart). 1 out of 5 athletes will have enlargement in the left atrium (the other major chamber on the left side of the heart). Even the thickness of the muscular walls of the left ventricle will increase by 10-20% in well-trained athletes; however, in the majority of athletes, absolute wall thickness will still remain within the normal spectrum by adult standards.
ATHLETES’ RISK OF SUDDEN CARDIAC DEATH
I don’t want to bore you with too many scientific analyses, but here’s one that best summarizes the challenges before us. In a 10-year study of United States (U.S.) collegiate athletes, 182 deaths were found to have occurred, or the equivalent of 18 athlete deaths per year. Six of the deaths each year were related to a likely or probable heart or arterial blood vessel (cardiovascular) abnormality, and it’s these people that I believe we can save. You tell me that it’s only six people, but that’s just at the college level. There’s 15 times more U.S. athletes participating annually in high school varsity activities. Besides, if you or your child happened to be one of these athletes, it suddenly matters a million times more.
In the previously mentioned study, the most common cardiac condition to be associated with an athlete’s sudden death was hypertrophic cardiomyopathy, and this disease process was felt to be causative in one-third of all cardiovascular deaths (21 total). (Hypertrophic cardiomyopathy is a genetic condition resulting in abnormal thickening of the walls of the left ventricle.)
Other causes included abnormal development of the arteries supplying blood to the heart, which is called congenital coronary anomalies (8 deaths), and the development of blockage in the heart arteries, known as coronary artery disease (5 deaths). Rupture of the major artery in the chest called the aorta (3 deaths), a genetic condition resulting in fibrous or fatty tissue deposits in the heart, known as arrhythmogenic right ventricular cardiomyopathy (3 deaths), enlarged heart conditions, known as dilated cardiomyopathies (2 deaths), inflammatory heart conditions, known as myocarditis (2 deaths), and an electrical heart problem, known as Long QT Syndrome (1 death), were some of the other causative factors.
THE CHALLENGES WITH ATHLETES AND SCREENING
There is not a universally accepted definition for athlete. A person who engages in “routine vigorous physical exercise in the settings of competition, recreation, or occupation” is a workable proposal by one group of experts, but for the purposes of medical screening, there remains no question that a true athlete is an outlier from the rest of the population. Consider the following:
The inherent nature of competitive athletes is to show no weakness. They are pushed by themselves and often a multitude of outside forces (e.g., parents, coaches, teams, and athletic associations) to perform at the highest level. They are trained to fight through pain and are coached to never give up, never slow down, and even occasionally, to succeed at all costs.
Despite the numerous longterm benefits of regular physical activity, there is a paradoxical, but small, risk of sudden cardiac arrest (SCA) and/or death (SCD) associated with exercise. Athletes routinely find themselves in the summer heat, wearing a rubber suit, running sprints with a parachute tied behind them for resistance. From the standpoint of the heart, they might as well be Navy Seals. This group of people is not your average one by any standpoint. It only makes sense for special rules to apply.
The major obstacle proposed to screening athletes in this country is cost. But, I’ll tell you below why that argument makes less sense. More reasonable considerations include the overall low prevalence of cardiac death in this population, as well as imperfections of screening studies and the impact of false-positive testing (situations where an abnormal screening test ultimately does not result in any concerning pathology being found). Finally, somewhat amazing to me, we still don’t have robust data evaluating the benefits of screening in this population. In fact, a “think tank” of experts was assembled recently to jumpstart future research and collaboration in this area. I’ll be anxious to see what materializes, but one thing is for sure now: our current guidelines regarding pre-participation screening of athletes are an outdated experiment. Just keep reading.
CURRENT U.S. AND EUROPEAN GUIDELINES REGARDING ATHLETIC SCREENING
For athletes under 40 years of age, the U.S. guidelines (American Heart Association), last updated over seven years ago, recommend that an athlete (1) have an assessment of personal and family history, and (2) undergo a physical exam. That’s it. Then, good luck to you climbing into a sauna wearing a rubber suit with a parachute. Never mind that the history and physical exam described above have been known for nearly twenty years to only detect 3% of lethal cardiovascular abnormalities in this patient population.
European guidelines, last updated over nine years ago, actually make an attempt to improve on the obvious limitations of the history and exam and recommend adding a mandatory ECG (electrocardiogram) to the athlete’s assessment. An ECG is a non-invasive test that takes minutes to perform and interpret. For those not in medicine, it’s those squiggly lines on a piece of paper that represent the electrical activity of the heart. The final result kind of looks like what you might see on one of those lie detector tests, with a marked fluctuation in activity during every heart beat.
A potential benefit of obtaining a mandatory ECG is that the most common condition (hypertrophic cardiomyopathy) attributed to sudden cardiac death in athletes results in an abnormal ECG in up to 95% of cases. Maybe, we can catch some of these. Indeed, one Italian study showed that the annual incidence of sudden cardiac death in athletes decreased by 89% once mandatory screening, to include a standard ECG in everyone, was initiated. Another study, making the generous assumption that this same data could be extrapolated to the U.S. population, estimated that 4,813 athlete lives would be saved over 20 years by implementing a similar ECG screening program for all athletic participants. Those numbers make an ECG seem like an obvious thing to be doing. But, why doesn’t the American Heart Association agree with the European Society of Cardiology guidelines and recommend screening U.S. athletes with ECGs? The first answer is cost.
THE COST OF ECG SCREENING
We live in America in 2014, and our healthcare focus has suddenly become nine-parts cost and one-part innovation. Everything has become an Affordable Care Act (or “Obamacare”) issue. Trust me, this should not be one of them, and I’ll get to more on that later.
The same study previously mentioned, which notes that nearly five thousand U.S. athletes may be saved over two decades, also claimed that saving those lives through mandatory ECG screening would cost over $51 billion. Say what? I did not mistype that. And, that’s just a minimum of $51 billion. The article estimated that it just might be as much as $69 billion, or $14.4 million per one life saved! For an ECG?
First of all, you should know that medial studies are historically riddled by fuzzy math, so when I read the article and came across that ridiculous sounding number, I immediately called shenanigans, which in my state of Texas is the same as saying: “Ain’t no way.” $51 billion sounds like someone miscalculated a few zeros, especially when the cash price for a single ECG in my own office is a mere $18.
As you might expect, truth is usually best found in the details, and I’m about to reveal those to you. But, the amazing fact is that I’ve seen the conclusion of this article used a number of times to argue against ECG screening in U.S. athletes. Its summary comes up routinely in debates within my own medical professional societies. And, its conclusion is nowhere close to being accurate.
THE REAL COST OF ECG SCREENING
The article that I’ve been referring to above is titled: Preventing Sudden Death of Athletes With Electrocardiographic (a.k.a. ECG) Screening. Given that the article is clearly supposed to be about ECG screening, you will be very interested to know how the cost of ECG screening is being calculated by the article’s authors. In fact, what makes up $38 billion of the estimated $51 billion minimum cost has absolutely nothing to do with an ECG. This is the cost estimated by the authors for each athlete to obtain a history and physical exam, something that I already explained to you is all of 3% helpful. Extrapolated another way, if you want to only be helpful to 3% of the estimated nearly five thousand potentially preventable athletic fatalities over the next 20 years, spend $38 billion. Interestingly, this is precisely what the currently outdated U.S. guidelines are telling us that we should already be doing now anyhow. Allow your family physician or even chiropractor (as many states do) to sign off on an athlete’s physical, and you might save one athlete’s life by spending $264 million on history and physical exams. This, like the U.S. guidelines, makes essentially no sense, but counting the cost of these history and physical exams against an ECG screening process is absolutely ludicrous.
The fuzzy math, however, gets even worse. The article assumes one ECG to cost $39. This is just medical funny money, and if you’d like to understand more about how physician businessmen and businesswomen can reduce healthcare costs, read Chapter 9: Restoring Value to Healthcare in my book. Regardless, you can find the cash prices of medical testing in my specialty clinic here, but an ECG, like I previously mentioned, is $18.
A handful of people will have an abnormal ECG, and the article above seeks to estimate additional medical costs that might result from widespread ECG screening. For example, an echocardiogram (or heart sonogram that uses sound waves to obtain real-time images of the heart) might be required to further evaluate an abnormal ECG, and the article assumes the cost of an echocardiogram to be $754 in its calculations. But, this isn’t the real cost of an echocardiogram. In fact, if you allow me, and not the hospital, to manage the overhead for this study, you will spend only $199. The same is true for an exercise treadmill test ($249 vs. $83 in my office) and so on.
In fact, the real cost for ECG screening is less than one-tenth the amount that this article surmises. Rather than a minimum of $14.4 million for one life-saved, the figure is actually closer to $1 million. Moreover, in medicine, we don’t routinely judge cost-effectiveness by a cost per life-saved metric. Instead, we measure value by determining the cost for one quality-adjusted life year (QALY). For example, a year of life lived in perfect health is worth one QALY.
Dialysis, for over a decade, has been viewed as the gold standard for comparing the cost-effectivenesss of various medical therapies. Dialysis involves the continued artificial support of a patient’s kidney function after the patient’s own kidneys have failed. Dialysis adds years to a person’s life, and the current cost of dialysis is about $100,000 per QALY.
As examined above, ECG screening as an intervention could save athletes at an estimated cost of $1 million per life-saved. These athletes will typically be saved at young ages and therefore maintain the possibility of an extended lifespan. Even if you conservatively estimate that a young athlete will only live an additional 20 years of life because of the screening process, the cost of ECG screening would be about $50,000 per QALY. Not only is this amount markedly less than the well-established standard of dialysis, it is one-third the sum that the World Health Organization typically uses as an acceptable benchmark (e.g., $150,000 per QALY).
Indeed, cost is much less of an issue when you analyze ECG screening appropriately. We are arguably already spending more money for less value on numerous other medical therapies.
THE PROBLEM OF FALSE-POSITIVE SCREENING TESTS
The most legitimate reason that the U.S. guidelines do not currently recommend ECG screening deals with concerns for false-positive results. The term “false-positive” refers to the situation where a particular test ends up being abnormal, yet after additional assessment (usually with more tests), no concerning disease process actually exists. False-positive rates exist in various degrees for all medical tests, mainly because there’s usually never a perfect study to evaluate people.
Using standard adult criteria, ECGs can show abnormal findings in up to 40% of certain endurance athlete populations. The rate of false-positives is improved when experts more familiar with evaluating athletes incorporate athlete-specific ECG criteria for normality. (For example, one such modification of ECG criteria, known as the Seattle Criteria, with contributions from both European and U.S. experts, has resulted in improvements regarding ECG interpretation in athletic populations.)
But the truth is that false-positives will always exist. We are talking about a screening test, and a screening test is always going to identify some people without any problems because the main goal of the screening test is not to miss anybody that could have a lethal problem. For this very reason, dealing with false-positives becomes an educational process for all involved and a cultural understanding of what a positive test may or may not even mean.
Extrapolating from the Italian study mentioned above, for every 100 athletes undergoing ECG screening, nine of them will have an abnormal tracing and likely will need to undergo additional testing. This doesn’t mean that these nine athletes won’t be able to play. They will just need a more thorough assessment. Once this process is better understood for all athletes, less anxiety will exist over time from abnormal results, and ultimately athletes will begin to recognize the system’s focus on individual safety.
Finally, keep in mind that false-positives, as mentioned above, are not unique to ECG screening measures. In fact, the history and physical exam (the only interventions currently supported by the U.S. guidelines) aren’t the least bit better in this regard, and may actually result in more false-positives than ECGs. In fact, one study suggested a 50% false-positive rate using the history and physical exam alone, while ECG screening actually faired better. The main conclusion that you can take from all of this is that regardless of the intervention, whether that be (1) history and exam or (2) ECG, both seem to be insufficient by themselves.
THE BENEFIT OF COMBINING ECG WITH ECHOCARDIOGRAPHY
A recent study of high school athletes undergoing screening evaluation with (1) standard history and physical exam, (2) ECG, and (3) echocardiogram, identified nine concerning medical disorders. Five of those disorders were potentially lethal abnormalities, whereas the other four were felt to be non-lethal but still requiring of medical follow up. Standard history and physical exam was able to pick up on four of the nine disorders (a 44% identification success rate). By now, I suspect that this isn’t surprising to you. I’ve been showing you study after study outlining the limitations of our history and physical exam for screening purposes. In fact, I suspect that you are somewhat amazed that the history and physical exam did as well as they did in this study. Yet, at the end of the day, the screening method recommended by U.S. guidelines missed almost two-thirds of the lethal abnormalities in these athletes.
There is something, however, that is more intriguing about this study. Echocardiography was performed. Echocardiography uses sound waves to gather vast information about the heart and surrounding structures in a non-invasive way. Echocardiography uses no X-rays, exposes patients to no radiation, and the technology requires no contrast dye. Echocardiography is well known to be able to improve on both the sensitivity and specificity of ECG screening. Regardless, you will be interested to know that when grouped together in this study, ECG and echocardiography identified all nine of the disorders (a 100% success rate), including every lethal one.
THE RDB4P GUIDELINES
The U.S. guidelines for screening athletes clearly need to be re-written. In fact, the current paradigm built around the history and physical exam should be abandoned. This is no longer medicine in the 1880s. Staring at an asymptomatic patient’s neck veins (part of the physical exam) makes little sense anymore. It provides a single color of paint to a clinical portrait that would have long sense been completed by the information obtained from an echocardiogram. In many ways, out of some paradoxical matter of principle, we continue to travel across the country by horse and buggy despite the fact that we have our own jet. It’s time the wiser physician community sitting around thinking up guidelines accepts this inevitable transition in medicine. We’ve been fighting this for too long.
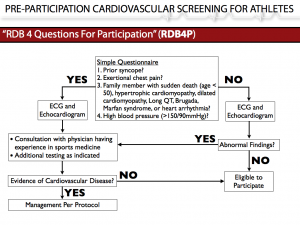
So, I present to you the first thing in a long time that actually makes some sense regarding pre-participation cardiovascular assessment of our elite athletes. For now, let’s call it RDB (my initials, but you can put your own there, I don’t care) 4 Questions For Participation Guidelines. Then, since that’s too wordy for headlines, let’s shorten it to RDB4P. It’s nothing revolutionary. It’s like selling common sense. And, you might study it with more gusto and find that this algorithm isn’t any good either. But, at the very least we’ll advance ourselves by moving away from our current state of clear futility regarding the athletic screening process. My late grandfather once told me that there comes a time when you will just need to put your paddle in the water and start going somewhere other than where you’ve been. I can’t say it any better myself.
The hallmark of RDB4P is that EVERY elite athlete gets both an ECG and an echocardiogram. The total cost of these two tests in my office is $217. Remember, this isn’t an Obamacare issue. This isn’t something for which the government should be responsible to pay. For the record, you will probably spend more than $217 on your kid’s baseball bat, glove, and helmet. Perhaps your athletic association will even cover the cost of screening with their own fees and budget. Keep in mind, we are talking about an athlete’s life that could be at stake.
A part of this algorithm (see below) is a simple 4 question survey that could be answered on an online website, at school, or at sign-ups for an athletic club team. If you answer “YES” to any of these questions, you automatically will get to see me (or another physician who focuses on the assessment of athletes). But, before you see me, you will undergo testing with an ECG and an echocardiogram. I’ll then have the opportunity to delve more into your clinical history while reviewing these studies. Concerns may be alleviated, more thorough testing might be required, or a clinical diagnosis might even be made with appropriate treatment initiated. Ultimately, your athletic status will be decided on not just by me, but in conjunction with me and all the parties involved, including yourself and the athletic association under which you are participating. My role is to provide medical education and a global assessment of risk such that informed decisions regarding your health can best be made.
If you answer “NO” to all of these four questions, you will still undergo screening with an ECG and echocardiogram. Both of these studies will be reviewed by me or someone like me, but you won’t have to see me if the composite review of those studies indicates no concerning findings. You will be cleared to participate. If your screening studies viewed together raise any red flags, then you will undergo a more thorough evaluation as outlined above.
It’s game over for the U.S. guidelines. A simple schematic outlining the RDB4P algorithm is found below.