I’m going to tell you the real goal for a clinical trial in medicine these days.
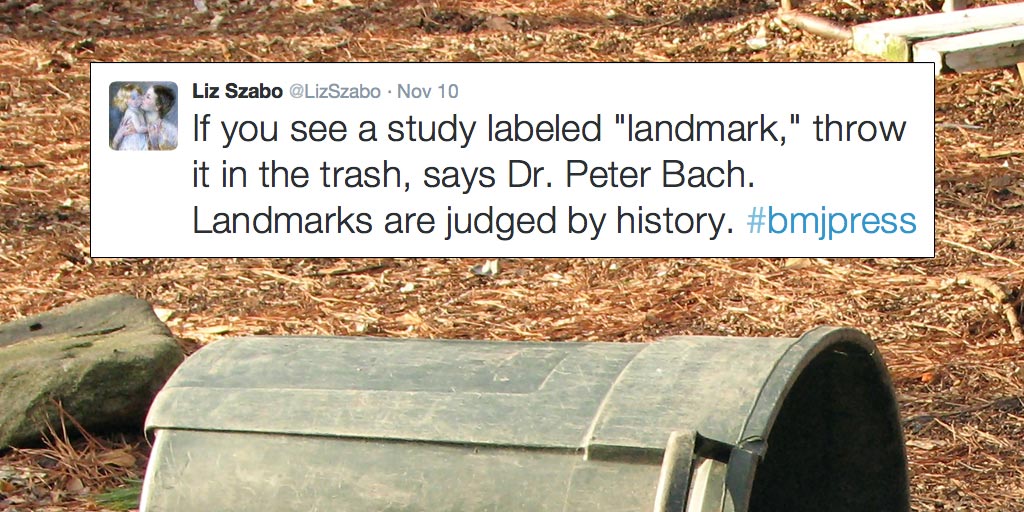
It’s to be landmark.
It’s what the trial sponsors seek and their investigators envy.
Landmark is the ultimate goal.
In fact, trial sponsors will frequently call their own study landmark even before it gets published in a scientific journal. Kind of like getting your Super Bowl ring fitted during the preseason.
The sponsors of a recent blood pressure study, known as the SPRINT trial, did just that. And, just this week, their self-awarded landmark study was finally published for all to review.
I previously told you whether or not you should take more notice of your blood pressure at home, so I feel a brief discussion about this trial might also be helpful.
THE SPRINT TRIAL
The SPRINT trial enrolled over 9,000 people in the United States and Puerto Rico. For every patient enrolled, there was general consensus that the patient needed to be taking medication for high blood pressure.
I’ll say that again.
Everyone in the trial, without question, was felt by medical personnel to require blood pressure medication. Therefore, this wasn’t a trial of if you needed blood pressure medication. It was essentially a trial of how much.
Patients were divided into two groups based upon systolic blood pressure (SBP) goals. One group was given an intense target (SBP less than 120mmHg). The other group was given a standard, or less-intense target (SBP less than 140mmHg). Of note, no patients with diabetes or prior stroke were enrolled.
The trial was stopped early, at a median follow up of just over 3 years. Like I told you, the trial was landmark. Statistically, the investigators said the results were clear, and that the trial need not to be continued any longer.
The intense blood pressure group won.
As you might have expected, the intense group required more medications to get their results. On average, each patient needed one more medicine (a mean of 2.8 versus 1.8 blood pressure medications, respectively, between the two groups).
By adding (on average) one more medication per patient, the mean blood pressure of the intense group was 13 points lower than the less-intense group (121.5 mmHg verses 134.6 mmHg, respectively).
And, as I told you, the intense group, with the lower average blood pressure readings, won. Their primary outcomes were better. How better? I’ll let you decide.
1) The intense group had less deaths.
But, there is something you must know.
For 98.5% of the patients enrolled in the study, it did not matter to what group you were assigned. Intense or less intense therapy was inconsequential to you dying. For 98.5% of the patients in either group, this outcome was the same. Regardless.
2) The intense group had less heart failure.
But, again, here is what you should know.
For greater than 99% of the patients enrolled, the group assigned didn’t matter when it came to developing heart failure. What was going to happen, just happened. Anyway.
3) The intense group had more patients suffer from serious adverse events like too low of blood pressure (hypotension), passing-out spells (syncope), and sudden kidney injury (acute renal failure).
But, yes, you already know.
For 99%, 99%, and 98% of the patients, respectively, these events occurred with the same frequency no matter which of the group’s average number of pills you were receiving.
I could go on and on. In fact, there were many more intriguing statistical findings. For example, the lower your blood pressure was at the beginning of the trial (e.g. if you were in the subgroup of people with a “seemingly decent” SBP ≤ 132mmHg at the start), the more numerical benefit you received regarding the primary outcome by making your blood pressure even lower on intense therapy.
But, lower, lower, lower, wasn’t even obtainable most of the time. That’s right. The intended target for the intense group (SBP < 120mmHg) wasn’t even achieved in over half the patients. In these people, the target was really nothing more than a theoretical construct.
As for how any of this might apply to an individual patient outside of this trial is really anyone’s guess. All we’ve really established are the averages of this and that, and apparently, these may be irrelevant for nearly every end-point examined in about 99% of the people involved.
But, again, this is what we call landmark.
And, by saying that word, we almost succeed at dodging the real question:
What are you, the patient, to do about your blood pressure?
Well, I’ll tell you what I intend to do with mine.
I’ll entrust it to a doctor. A doctor who knows that science and technology alone will never define my best course of action. A doctor who, as Dr. Michel Accad has previously stated, understands Mutton’s Law of optimal patient care. Basically, someone who…
…knows what to do and when to do it.